We found 70 results for EFM

EFM Advanced #01: Terms & Guidelines Part 1
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the first of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
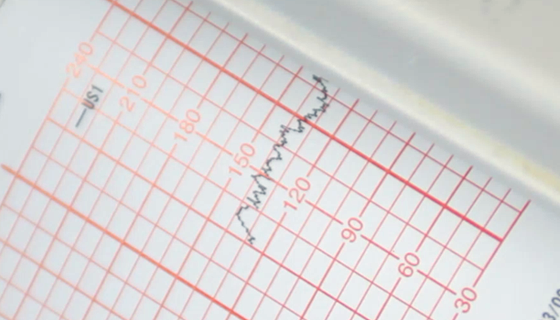
EFM Advanced #02: Terms & Guidelines Part 2
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the second of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
EFM Advanced #03: Physiology & Pathophysiology Part 1
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the third of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #04: Physiology & Pathophysiology Part 2
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the fourth of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #05: Interventions & Management Part 1
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the fifth of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #06: Interventions & Management Part 2
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the sixth of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #07: Interventions & Management Part 3
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the seventh of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced #08: Interventions & Management Part 4
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the final of an 8-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced Modules 1 & 2 (FL)
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the first of a 3-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
EFM Advanced Modules 3 & 4 (FL)
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the second of a 3-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.

EFM Advanced Modules 5-8 (FL)
EFM diagnostic error and miscommunication are major causes of perinatal morbidity and mortality, as well as, malpractice claims. Use of the 2008 NICHD terms and guidelines creates a standardized framework for interpretation while reducing errors and omissions. This activity is the third of a 3-part series that applies NICHD principles into critical thinking activities to improve retention of key concepts in EFM interpretation.
.png?access_token=DKH1woIy1kRFYdz63VBSFLjkdn02SCkztIWLpBpP)
EFM Case Study #01: OP Malpresentation
Occiput posterior (OP) malpresentation occurs 5-12% at birth, increases risk of surgical birth, and frequently coincides with category II or III FHR patterns. In an effort to reduce cesarean births, ACOG and SMFM guidelines encourage practitioners to perform manual rotation of the fetal occiput during the second stage of labor while AWHONN encourages use of various birth positions for spontaneous rotation.
.png?access_token=DKH1woIy1kRFYdz63VBSFLjkdn02SCkztIWLpBpP)
EFM Case Study #02: EFM Triage, Part 1
This activity provides an EFM Triage model for swift and accurate EFM interpretation when there is no clinical information about the mother or her pregnancy.
.png?access_token=DKH1woIy1kRFYdz63VBSFLjkdn02SCkztIWLpBpP)
EFM Case Study #02: EFM Triage, Part 2
This activity provides practice using an EFM Triage model for swift and accurate EFM interpretation when there is no clinical information about the mother or her pregnancy.
.png?access_token=DKH1woIy1kRFYdz63VBSFLjkdn02SCkztIWLpBpP)
EFM Case Study #02: Modules 1 & 2 (FL)
This activity provides an EFM Triage model for swift and accurate EFM interpretation when there is no clinical information about the mother or her pregnancy.
We found 3 results for EFM
-
Education
Section: MI Public Website -
Assessments
Section: MI Public Website -
Course Packages
Section: MI Public Website

